Superior Surgery
In the hazy world of Internet postings and braggadocios marketing, often it is difficult for the patient unfamiliar with spine surgery or surgery in general to discern between what is good and what is truly superior surgery. However, there are certain specific OR techniques and general principles, which one can follow to increase the likelihood of a good outcome and patient safety.
Going the Extra Mile for Excellence
Outcomes
The Diagnosis
The Surgeon
**Note to Lumbar ADR Patients: Prof. Dr. Bertagnoli uses the retroperitoneal approach to the spine with an adhesion barrier to prevent the vasculature from adhering to the adjacent tissues, which makes revisions difficult if not impossible. He does not recommend the much quicker transperitoneal approach, as the risk of infection and other complications are unacceptable. We know of at least one surgeon who switched from the transperitoneal to the retroperitoneal approach, but does not use an adhesion barrier, claiming it is not necessary. This is not good news for his patients, who may need another anterior spine surgery in the future, as the lack of an adhesion barrier carries the risk of exsanguination ( excessive blood loss causing death).
GOING THE EXTRA MILE FOR EXCELLENCE:
What does this mean in practical terms? Prof. Dr. Bertagnoli’s willingness to go the extra mile for excellence is demonstrated in many ways. For example:
In ADR surgery, surprisingly many well-known, aggressively-marketed hospitals and surgeons do not use a fluoroscope to align the ADR in the precise center of the vertebrae (aligned with the anterior posterior midline from the coronal or face-on view), nor do they identify the correct placement (fore and aft from the sagittal or side view). This disregard for the improved accuracy obtained by fluoroscopy also occurs in fusion surgery.
Of course, Prof. Dr. Bertagnoli always uses a fluoroscope, as correct alignment is absolutely critical to the success of the operation. There is normally only a 1.5 mm tolerance in a single level surgery on each side of the vertebrae, sometimes less depending on the device.Tolerance levels for alignment error go down radically in multilevel surgery.
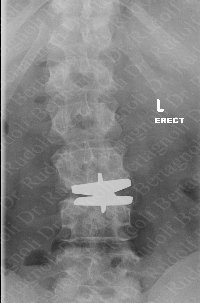
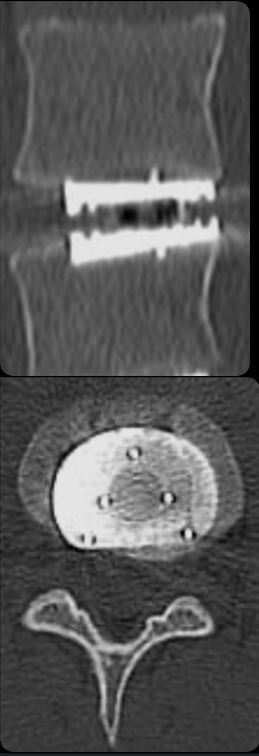 Without proper ADR alignment, the resulting imbalance of the spine creates bio-mechanical stresses that can cause facet joint problems as well as back muscle adaptation from constant compensation. Unfortunately, the patients of these surgeons often require revisions, such as the patient in the image showing an example of a misaligned and misplaced ADR stressing the entire spine. Fortunately in most cases a dorsal stabilization can be done to remedy the situation, and Prof. Dr. Bertagnoli will do revisions on these patients, but would have preferred to do it correctly the first time. If the misalignment is too great then a removal and replacement of the ADR may be necessary. In the case on the right, the ADR is rotated as well as misaligned. The lower plate of the ADR is also located too deeply in the bone. This case was done by another European surgeon. Please note also that this device does not have a robust keel, which offers more of an opportunity for migration after surgery.
Without proper ADR alignment, the resulting imbalance of the spine creates bio-mechanical stresses that can cause facet joint problems as well as back muscle adaptation from constant compensation. Unfortunately, the patients of these surgeons often require revisions, such as the patient in the image showing an example of a misaligned and misplaced ADR stressing the entire spine. Fortunately in most cases a dorsal stabilization can be done to remedy the situation, and Prof. Dr. Bertagnoli will do revisions on these patients, but would have preferred to do it correctly the first time. If the misalignment is too great then a removal and replacement of the ADR may be necessary. In the case on the right, the ADR is rotated as well as misaligned. The lower plate of the ADR is also located too deeply in the bone. This case was done by another European surgeon. Please note also that this device does not have a robust keel, which offers more of an opportunity for migration after surgery.
In the example to the right we see the same problem of coronal imbalance developed from misaligned cervical implants. Initially, patients may feel no or little pain with this misalignment. However, it is very likely that the increased stresses put on the muscles will eventually lead to pain and facet problems. In this image we can see the beginning of the misalignment of the spine. Facet problems are more likely to occur when deviation from the anterior and posterior midline occurs.

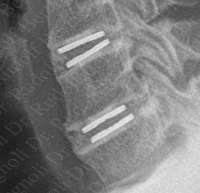
The margin of error in ADR surgery is quite small especially in multiple-level ADRs and even smaller in the cervical spine. Possibly 1 mm in any direction The next example shows two ADRs placed too far posteriorly by a German doctor. Additionally too much of the endplates of the vertebrae have been removed causing subsidence. The result is a coronal imbalance and subsequent autofusion. Results like this are difficult to revise (an anterior fusion will be necessary in this case) and revision offers significant risk to the patient, especially if the surgeon did not use an adhesion barrier. This is why doing it right the first time is so important. There is simply no substitute for experience and talent.
Although not shown here, we take this opportunity to say, the keyway for ADR should never be chiseled in the cervical spine. This represents a severe risk to the patient's safety and there has been reported at least one very serious accident using this technique. The keyway should always be drilled or sawed for precise control in the cervical spine. Of course, Prof. Dr. Bertagnoli uses a drill in the cervical spine for the keyway of the ADR.
Then the ADR is gently tapped in.

In the next example we see a misplaced fusion screw, which severely damaged the disc that it penetrated . Fortunately, in this case Prof. Dr. Bertagnoli was able to repair and remodel the damaged vertebra and replace the damaged disk..

Here we see a hybrid construct, that is a fusion in combination with ADR. These segments require significant engineering to prevent the pseudolisthetic, a (“slipped”) position, also called a subluxation. This subluxation will stress facet joints. It will also narrow the neuraforamina of that level to impinge the nerves that should have been liberated during the surgery. This patient remains in pain and is considering revision with Prof. Dr. Bertagnoli.
Proper sizing of the ADR is critical for success. The ADR is sized based on the height, width and angle of the normal position of that level of the spine. Most errors that we see come result from inadequate width of the ADR. The plates of the ADR should nearly cover the endplate of the vertebral bodies . This helps to prevent subsidence of the endplate into the vertebral body, and autofusion, which occurs when osteophytes grow around the ends of the ADR. The image on the right shows autofusion, where osteophytes have grown around the ADR and now the patient's neck is frozen. This was done by a well-known and aggressively marketed hospital. Prof. Dr. Bertagnoli will perform revision in these cases. This patient is now doing well after an eight hour revision surgery.

Careful removal of debris is an indication of good surgical technique. Too often we see the debris from previous surgeries causing complications. Surgery is not a race, where the doctor who finishes first wins. The surgeon must remove all material from the discectomy and vertebral remodeling. In the poor but instructive MRI on the right we see debris from a previous surgery impinging on the spinal canal. Again this was performed at a well-known and aggressively marketed hospital..
In ADR surgery, he spends more than the standard OR time in remodeling of deformed and diseased vertebrae. This is tedious work but it must be done to ensure no osteophytes are left to compress the nerves and in some cases the angulatures of bone endplates are correct.
The importance of applying bone wax to remodeled bone or ADR preparation sites cannot be over emphasized. The bones see these areas as damaged and will grow osteophytes in these areas to protect themselves. Application of bone wax to ADR preparation sites in the bone or remodeled areas of the bone helps prevent osteophytes from forming.
Prof. Dr. Bertagnoli preserves the anterior longitudinal ligament between the vertebrae whenever possible. He does this by cutting a window in the ligament and placing the ADR through the window. When complete he sews the window shut. The ligament heals and is preserved. Some surgeons believe that this ligament is not relevant and take no measures to preserve it.
Dexa bone scans help to assess the quality of bone, and all ADR surgeons should use this procedure, but many do not. Some only use it when there are obvious indications, such as the sex and age of the patients. (Indeed, Prof. Dr. Bertagnoli has discovered that men ( often ?) have lower bone densities than expected). Although there is approximately a 20% error rate (that is, a 20 % chance of a false positive and a false negative), the Dexa T-score is a good indicator of bone strength. Prof. Dr. Bertagnoli also makes perioperative judgments about bone quality during surgery. Weak bones can be made ready for ADR surgery with AMP vertebroplasty, which is an injection of bone cement into the bones. AMP vertebroplasty must be done with great care, as it is not without risk.
Many ADRs have keels that provide immediate lateral stability and that develop a stable bond to the trabecular or spongy bone. This makes the degree of congruity between the ADR endplates and the vertebra less critical, which minimizes the amount of bone remodeling required to permit stable implant fixation to occur. The benefits are twofold; avoiding subsidence of the ADR, and minimizing osteophyte growth. These ADRs require drilling or sawing of the keyway for the keel. Drilling is the safest method. This keyway must be checked for debris before the ADR is tapped in. It cannot be assumed to be clear. Checking the keyway should be part of any ADR surgeon’s procedure. Serious injury can happen and has happened in patients where this has not been done..
In ADR surgery, Prof. Dr. Bertagnoli spends more than the standard OR time in remodeling of deformed and diseased vertebrae. This is tedious work but it must be done to ensure no osteophytes are left to compress the nerves, and in some cases, that the angulatures of the bone endplates are correct..
ADR surgery, he has the patients wear an orthesis ( soft collar) after surgery , because he knows from research that up to 5% of patients can have a migration issue due to severe movements after surgery. Not so in his patients. This is particularly important at night, when people can thrash about in their sleep.
In ADR surgeries, he packs the surgery site between and around the vertebrae with anti-thrombin agents to effectively inhibit thrombin-induced fibrin formation and platelet aggregation.
In ADR surgeries, he has established approach protocols. For example, in L5/S1 only ADR surgery, the surgeon should enter from the right.
In ADR surgeries, he is chiefly responsible for the design of the implementation tools.
The removal and the controlling of bleeding makes for a better healing process and less of a scar. This takes time and care. Most of this work is done during the incision and approach. In all surgeries, he uses the latest effective tools and equipment to ensure a better outcome.
In Dorsal Pedicle Implants (DPI), he splits the muscles rather than cut them and remove them from the bone, which is the normal method. This is done with one exterior incision and two interior incisions. Of course, this makes the recovery for the patient much easier.
In Dorsal Pedicle Implants (DPI), again we see many hospitals and doctors not using fluoroscopes in this procedure, which have led to many terrible mistakes.
The removal and the controlling of bleeding makes for a better healing process and less of a scare. This takes time and care. Most of this work is done during the incision and approach.
Does this cost a little more? Of course, but a little more cost should not dissuade us from excellent medical treatment. After all, we only have one back.
OUTCOMES:
Many doctors claim to be the best in their fields. Look for peer reviewed scientific articles about surgical outcomes to prove a doctor’s claims. Look for data gathering by the doctor after the surgery, to see if the doctor is engaged in scientific studies.
THE DIAGNOSIS:
Every good surgical outcome begins with a good diagnosis. Every intervertebral disc space and sometimes each bone of the spine should be analyzed independently and with respect to the entire spine. If surgery is required, the surgeon should have mastered the broadest spectrum of viable surgical options that are appropriate for a which can apply to patient’s condition, and he/she should know how and when to apply them. Application of that treatment by the surgeon must be done with greatest attention to detail and organization as possible. Although the patient's awareness is due to the nerve impingements and the consequential pain, the underlying problems of the spine are almost never solely neurological, but mechanical. Therefore, the an understanding of the mechanical forces at play is critical to the development of a comprehensive, modern treatment plan and its application .
THE SURGEON:
The foreign patient should know that Prof. Dr. Bertagnoli always performs the operation. The operation is never delegated to another surgeon.
The surgeon, of course, is the key factor. One must look at the training and experience of the surgeon. Academically, one should also look for a surgeon, who publishes peer reviewed scientific articles about the techniques he/she is employing. If the surgeon is teaching the techniques to other surgeons, then you can be sure he is the intellectual and surgical master of his profession. And I the modern world of spine surgery a mechanical engineering background is a plus benefit for the doctor and his patients.
Historically, spinal surgery had only a very restricted set of techniques available (basically discectomy and dorsal fusion) – hence only obtuse solutions were available to the patients. However, with the advent of so many new technologies for the spine, this is no longer the case. Each intervertebral disc space must be analyzed for the best solution for that intervertebral space. Therefore, the patient should be seeking a surgeon who has experience with all the new and proven techniques such as : artificial disc replacement, zero profile fusions, dynamic stabilization system, interlaminar decompression, discectomy with Barricaid and so on. Fortunately, Prof. Dr. Bertagnoli has been at the forefront of these technologies. His training as a mechanical engineer before he became a doctor has proven to be essential in the development of some of these technologies, but more importantly in the correct application of these technologies to the individual patient.
The superior surgeon must also be willing to reject new technology that which does not prove to be of benefit to the patient. Just because it is new, does not make it better. Also, a truly great surgeon must have superior manual skills in the OR. For the individual browsing the Internet Internet browser this is very difficult to determine know . Only references by experienced observers can help the patient select the doctor who possesses the level of manual dexterity that enables him/her to master the art of spine surgery.
HOSPITALS AND STAFF:
Before, during and after the operation the hospital and staff take excellent care of you. Members of that staff are include the anesthesiologist, nurses and physical therapist. Again, a wealth of experience with spine surgery patients is important for a good outcome.
